Ever wondered what does GERD feel like? If you’re experiencing a burning feeling in your chest or a sour taste in your mouth, it might be GERD. This condition involves stomach acid flowing back into the esophagus, causing heartburn, regurgitation, and chest pain. In this article, you’ll learn about these symptoms and discover ways to manage and relieve them.
Table of Contents
Key Takeaways
GERD is a chronic condition resulting from weakened lower esophageal sphincter, leading to frequent acid reflux that can cause serious health issues if untreated.
Common symptoms of GERD include heartburn, regurgitation, chest pain, difficulty swallowing, and a persistent sour taste in the mouth.
Effective management of GERD requires a combination of lifestyle changes, over-the-counter and prescription medications, and potentially surgical interventions for severe cases.
Understanding GERD and Acid Reflux
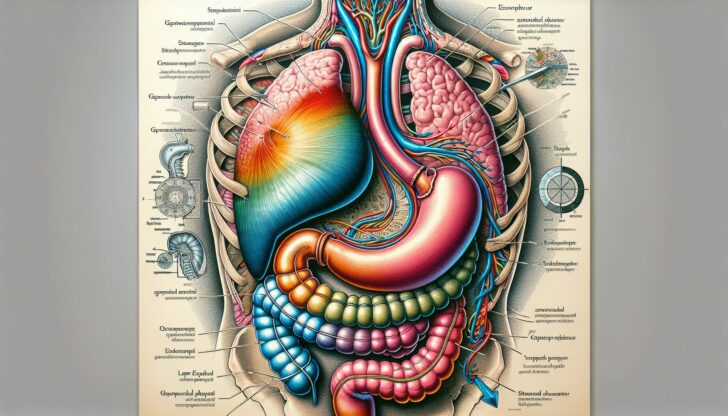
Gastroesophageal reflux disease (GERD) and acid reflux are related conditions, with GERD being the more severe form. Acid reflux involves the backflow of stomach contents into the esophagus, causing irritation and discomfort.
When chronic acid reflux occurs frequently, it is classified as gerd acid reflux, a more chronic and severe form of reflux that can lead to serious health issues if left untreated, including occasional acid reflux.
What is GERD?
GERD stands for gastroesophageal reflux disease. This condition occurs when the lower esophageal sphincter, a muscle at the junction of the esophagus and stomach, becomes weakened or relaxed, allowing stomach acid to flow back into the esophagus. If heartburn—a burning sensation in the chest—occurs more than twice a week for several weeks, it is typically considered GERD.
Various factors, including obesity, certain lifestyle choices, and some medications, can increase the risk of developing GERD.
How Acid Reflux Occurs
Under normal circumstances, the lower esophageal sphincter functions as a barrier to prevent stomach contents from entering the esophagus. However, when this muscle malfunctions, stomach acid can flow back into the esophagus, leading to acid reflux. This backflow can cause a range of uncomfortable symptoms and, if frequent enough, can result in the chronic condition known as GERD.
Common Symptoms of GERD
GERD is characterized by the recurrent return of stomach contents into the esophagus, often leading to frequent episodes of heartburn. The common symptoms of GERD include heartburn, regurgitation, and chest pain, each affecting individuals differently and varying in intensity.
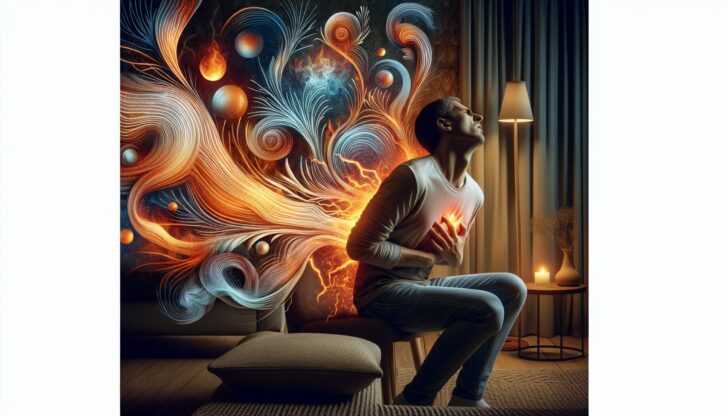
Heartburn
Heartburn, the most recognized symptom of GERD, is often described as a burning feeling in the chest that can extend to the throat.
This burning sensation typically occurs after meals or when lying down and is triggered by foods such as:
citrus fruits
tomato-based products
onions
garlic
chocolate
high-fat or spicy foods
Heartburn is a common experience, with at least 60 million Americans reporting it at least once a month. While antacids can provide quick relief by neutralizing stomach acid, frequent heartburn should prompt a visit to the doctor for further evaluation.
Regurgitation
Regurgitation is another common symptom of GERD and involves the sensation of food, liquid, or stomach acid coming up into the throat. This can result in a sour or bitter taste in the mouth, adding to the overall discomfort of GERD.
Regurgitation can occur at any time but is often more noticeable after eating or when lying down.
Chest Pain
Chest pain associated with GERD can be quite distressing and is often described as a non-burning sensation that may radiate to the back. This pain can feel like pressure or discomfort that lasts for several hours, mimicking the symptoms of a heart attack.
Given the serious nature of chest pain, it is crucial to seek immediate medical evaluation to rule out other potentially life-threatening conditions.
Other Symptoms of GERD
Beyond the common symptoms, GERD can manifest in various other ways, making it a complex condition to manage. These additional symptoms include a sour or bitter taste, difficulty swallowing, and chronic cough or sore throat.
Sour or Bitter Taste
A sour or bitter taste in the mouth is a frequent complaint among GERD sufferers, caused primarily by the regurgitation of stomach acid. This unpleasant taste often arises when stomach contents return to the esophagus and reach the throat, leading to a constant sour or bitter flavor that can significantly impact one’s quality of life.
Difficulty Swallowing
Difficulty swallowing, or dysphagia, is another common symptom of GERD. This condition can occur when chronic acid exposure leads to inflammation, scarring, or narrowing of the esophagus. The resulting discomfort or pain while swallowing can make eating a challenging task and may also indicate more severe complications such as esophagitis or ulcers in the esophagus.
Chronic Cough and Sore Throat
GERD can also lead to chronic coughing and a persistent sore throat, primarily due to acid irritation. A persistent cough, especially at night, is a common symptom and can be accompanied by throat soreness due to the continuous irritation caused by stomach acid.
Risk Factors for GERD
Several risk factors can increase the likelihood of developing GERD, ranging from lifestyle and dietary choices to medical conditions and medications.
Understanding these risk factors is crucial for effective management and prevention of GERD.
Lifestyle and Dietary Choices
Lifestyle and dietary choices play a significant role in the development and exacerbation of GERD symptoms. Common dietary triggers include chocolate, coffee, fried foods, and peppermint. Foods that are high in fat, spicy, or heavily processed can further worsen GERD symptoms.
Avoid lying down for at least two hours after eating and be mindful of dietary choices to minimize the risk of reflux.
Obesity and Pregnancy
Obesity is a significant risk factor for GERD, as excess weight increases pressure within the abdomen, making acid reflux more likely. Similarly, pregnancy can lead to hormonal changes that relax the lower esophageal sphincter, increasing the likelihood of acid reflux.
Both excess weight and pregnancy contribute to a higher risk of experiencing GERD symptoms due to increased abdominal pressure and hormonal changes.
Medications and Medical Conditions
Before: Certain medications and medical conditions can also contribute to the development of GERD. Hiatal hernia, a condition where part of the stomach bulges through the diaphragm, is a significant risk factor. Chronic conditions such as asthma, diabetes, and connective tissue disorders can also heighten the risk of GERD.
After: Certain medications and medical conditions can contribute to the development of GERD, including:
Hiatal hernia, a condition where part of the stomach bulges through the diaphragm
Chronic conditions such as asthma
Diabetes
Connective tissue disorders
Understanding these risk factors can help in managing GERD more effectively.
Complications of Chronic GERD
If left untreated, chronic GERD can lead to several serious complications, including esophagitis, Barrett’s esophagus, and respiratory issues.
These complications highlight the importance of managing GERD effectively.
Esophagitis
Chronic exposure to stomach acid can lead to esophagitis, an inflammation and irritation of the esophageal lining. This condition is primarily caused by frequent acid exposure and can result in painful swallowing and increased discomfort.
Barrett’s Esophagus
Barrett’s esophagus is a condition that arises from chronic GERD, where the cells lining the esophagus undergo changes that increase the risk of esophageal cancer. Repeated damage from gastric acid can lead to these precancerous changes, underscoring the need for vigilant monitoring and management.
Respiratory Issues
GERD can also lead to or exacerbate respiratory issues, such as worsening asthma symptoms and chronic cough. Acid exposure can irritate the bronchial tubes and lungs, leading to respiratory problems and highlighting the need for comprehensive GERD management.
Diagnosing GERD
Diagnosing GERD involves discussing symptoms with a healthcare professional and undergoing specific diagnostic tests. Accurate diagnosis is essential for effective treatment and management of the condition.
Symptom Discussion
A detailed discussion of GERD symptoms with a doctor is vital for an accurate diagnosis. Difficulty or pain swallowing, persistent cough, unintentional weight loss, nausea, vomiting, and bleeding require immediate medical attention.
If symptoms are frequent, severe, or unresponsive to over-the-counter medications, consulting a gastroenterologist is recommended.
Diagnostic Tests
Diagnostic tests for GERD include endoscopy, which allows direct examination of the esophagus and stomach, and pH monitoring to measure esophageal acidity levels over time. Additional tests like impedance-pH testing and high-resolution esophageal manometry help determine the type of reflux and assess esophageal muscle function, providing a comprehensive evaluation of the condition.
Treatment Options for GERD

Effective management of GERD often requires a combination of different treatment strategies, including lifestyle changes, over-the-counter medications, prescription medications, and surgical interventions.
Lifestyle Changes
Lifestyle changes can significantly reduce GERD symptoms. These include losing weight, eating smaller and more frequent meals, eliminating trigger foods, avoiding tight clothing, quitting tobacco, elevating the head of the bed, and avoiding meals at night.
Over-the-Counter Medications
Over-the-counter medications can provide quick relief for mild GERD symptoms. Common options include antacids, H2-receptor blockers, and foaming agents like Gaviscon®. Antacids neutralize stomach acid, offering immediate relief, while H2 blockers reduce stomach acid production but are less potent than prescription medications.
Foaming agents create a barrier on top of the stomach contents, preventing acid from refluxing into the esophagus.
Learn more, checkout Over-the-Counter Medications for GERD: An overview
Prescription Medications
In severe GERD cases, prescription medications like proton pump inhibitors (PPIs) are often used. PPIs are more effective than H2 blockers as they significantly reduce stomach acid production, offering longer-lasting relief.
These medications are typically used for long-term management of GERD symptoms and require a doctor’s supervision to ensure proper use.
Surgical Interventions
If lifestyle changes and medications prove insufficient, surgical interventions may be considered. Fundoplication, especially Nissen fundoplication, is the most common surgery for GERD, strengthening the lower esophageal sphincter to prevent acid reflux.
Other surgical options include the LINX® procedure, which involves implanting a magnetic ring to reinforce the sphincter, and endoscopic procedures for specific cases.
Summary
Understanding and managing GERD is crucial for maintaining a good quality of life. From recognizing common and other symptoms to identifying risk factors and exploring various treatment options, proactive management can prevent complications and improve daily comfort. If you suspect you have GERD, consult a healthcare professional for a tailored treatment plan. Remember, effective management often involves a combination of lifestyle changes, medications, and, in some cases, surgical interventions. Take control of your health and seek the relief you deserve.
Frequently Asked Questions
What does heartburn feel like?
Heartburn feels like a painful burning sensation behind your breastbone, often rising from your stomach and potentially spreading to your neck or throat. It is typically a discomfort stemming from the esophagus.
What are the 3 stages of GERD?
The three stages of GERD are mild, moderate, and severe. Mild GERD involves infrequent reflux, moderate GERD requires daily medication, and severe GERD indicates more significant complications.
What is commonly mistaken for GERD?
Heartburn is frequently mistaken for GERD, but conditions like gallstones, stomach ulcers, and esophageal cancer can also cause similar chest pain. It’s crucial to differentiate these symptoms for accurate diagnosis and treatment.
How is GERD diagnosed?
GERD is diagnosed through a detailed discussion of symptoms with a healthcare professional, alongside diagnostic tests including endoscopy and pH monitoring. Accurate diagnosis is essential for effective treatment.
What lifestyle changes can help manage GERD?
To effectively manage GERD, consider losing weight, eating smaller meals, avoiding trigger foods, and elevating the head of the bed. These lifestyle adjustments can significantly alleviate symptoms.