Imagine a world where technology could help treat medical conditions like epilepsy, depression, and stroke recovery. This is the power of Vagus Nerve Stimulation (VNS), a fascinating therapy that has shown promising results in various medical fields. Join us as we delve into the realms of VNS, exploring its benefits, applications, and side effects.
Table of Contents
Key Takeaways
Vagus Nerve Stimulation (VNS) is a therapeutic technique used to treat various medical conditions, including epilepsy, depression, and stroke recovery.
VNS carries risks and side effects. Its potential benefits can be maximized with proper preparation for the procedure.
Clinical studies have demonstrated encouraging results in treating these conditions but individual outcomes may vary.
Understanding Vagus Nerve Stimulation (VNS)
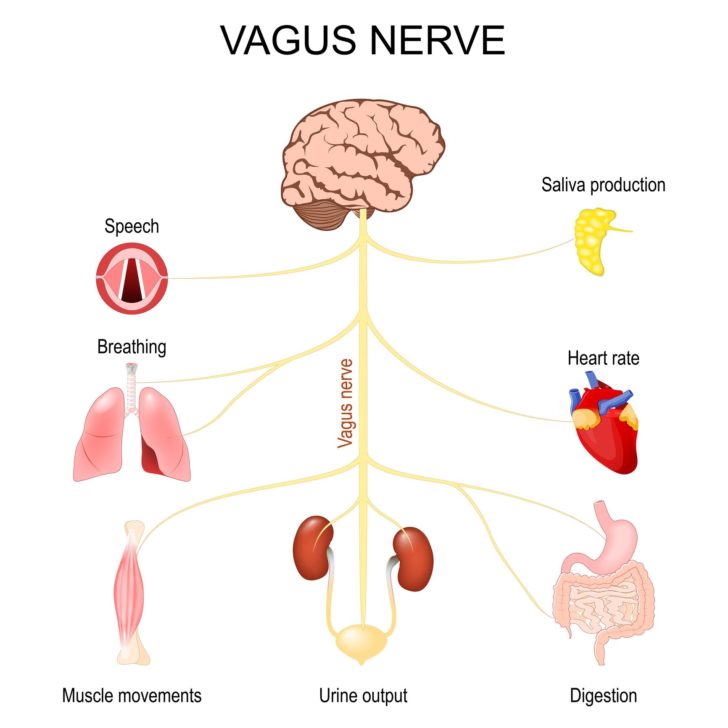
Vagus Nerve Stimulation (VNS), also called vagus nerve stimulation, is a therapeutic technique that uses electrical impulses to stimulate the vagus nerve, one of the most important nerves in the body, to treat various medical conditions, including chronic vagus nerve stimulation. This revolutionary vagus nerve stimulation therapy has its roots in the early 20th century when researchers began to investigate the influence of the autonomic nervous system on brain activity. Over time, VNS evolved into a surgical procedure involving the implantation of a programmable vagus nerve stimulation device to deliver electrical stimulation to the vagus nerve. Approved vagus nerve stimulation has shown promising results in treating various conditions. Non-invasive alternatives, like transcutaneous VNS, are also being explored, but their efficacy beyond small pilot studies remains uncertain.
The Food and Drug Administration (FDA) has approved VNS for specific applications, including the treatment of epilepsy, treatment-resistant depression, and stroke recovery. The application of VNS is versatile, with both invasive and non-invasive methods showing potential benefits in treating various conditions.
We will explore the different types of VNS and their applications for various medical conditions in the subsequent sections.
Invasive vs. Non-invasive VNS
Invasive VNS involves the implantation of a pulse generator device, which sends electrical impulses to the vagus nerve. Non-invasive VNS, also known as transcutaneous vagus nerve stimulation or vagal nerve stimulation, delivers electrical impulses through the skin rather than requiring surgical implantation. Both methods have shown potential benefits in treating various conditions, with pilot studies documenting the safety and tolerability of transcutaneous VNS for clinical indications such as epilepsy, depression, and pain.
VNS devices offer a range of programmable parameters, such as:
current charge
pulse width
pulse frequency
on/off duty cycle
These parameters can be customized to adjust the level of stimulation. Healthcare providers can adjust these parameters using a handheld computer and a programming wand placed on the skin over the device. This flexibility allows for the fine-tuning of stimulation to individual patient needs and the management of potential side effects.
FDA Approval and Applications
The FDA’s approval for certain applications of VNS has facilitated its widespread use in addressing diverse medical conditions. In the realm of depression, the FDA has approved VNS as a treatment for adults who have not seen an improvement in their symptoms after attempting other treatments. VNS has also been employed to address epilepsy and stroke recovery, with repeated vagal nerve stimulation being used to achieve therapeutic effects.
Despite its benefits, VNS therapy does come with some potential side effects, such as:
Voice alteration
Cough
Dyspnea
Dysphagia
Neck pain or paresthesias
However, these side effects can often be managed by regulating the electrical impulses and adjusting the stimulation parameters as needed.
Medical Conditions Treated with VNS
VNS has been used to treat a range of medical conditions, with varying degrees of success. Its ability to stimulate one vagus nerve opens up a world of possibilities for improving the lives of individuals suffering from conditions such as epilepsy, treatment-resistant depression, and stroke recovery.
In addition, ongoing research is exploring the potential of VNS in treating other conditions, such as Alzheimer’s disease, migraines, and cluster headaches. Subsequent sections will analyze how VNS has been applied to these specific medical conditions and the outcomes achieved to date.
Epilepsy
Epilepsy is a neurological disorder characterized by recurrent seizures, affecting millions of people worldwide. VNS has shown effectiveness in reducing seizures in patients with refractory epilepsy who do not respond to medications. It has been demonstrated to be efficacious in treating a variety of types of epilepsy, including partial seizures, simple-partial seizures, and epilepsy that is refractory to anti-seizure medications.
It is estimated that approximately 60% of epilepsy patients typically respond to Vagus Nerve Stimulation with a ≥50% reduction in seizure frequency. However, VNS is not recommended for epilepsy cases in young children or for seizures associated with Lennox-Gastaut syndrome (LGS). The effectiveness of VNS, therefore, depends on the specific type of epilepsy and the individual patient.
Treatment-Resistant Depression
Treatment-resistant depression is a debilitating condition that affects millions of people worldwide. VNS therapy has shown promise in improving mood and the quality of life in individuals with this condition. The rationale for investigating VNS as a treatment for depression is supported by preclinical and clinical studies, which have found that the vagus nerve has direct and indirect connections to the cortical-limbic-thalamic-striatal neural circuit associated with emotional and cognitive functions relevant to depression. Moreover, VNS has been found to affect the activity of neurotransmitters such as norepinephrine and serotonin, which are implicated in mood disorders.
Patients who undergo VNS therapy for depression may experience improved mood and quality of life. However, it is important to note that not all individuals with treatment-resistant depression will experience the same level of improvement. Factors such as the severity of the condition, the presence of comorbid conditions, and the specific type of VNS therapy used can all influence the effectiveness of the treatment.
Stroke Recovery
Stroke recovery and rehabilitation is a critical aspect of regaining function and independence following a stroke. VNS has been FDA-approved in combination with rehabilitation for hand and arm function recovery following an ischemic stroke. VNS rapidly activates key neuromodulators in the brain, such as the noradrenergic locus coeruleus and cholinergic nucleus basalis, promoting synaptic reorganization and enhancing plasticity in the motor cortex, leading to improved motor function and recovery after stroke.
Participants with moderate to severe arm impairment after ischemic stroke demonstrated clinically significant improvements in motor impairment and function with VNS therapy. VNS therapy paired with rehabilitation may lead to a greater improvement in distal upper extremity function in comparison to rehabilitation alone. This highlights the potential benefits of incorporating VNS into stroke recovery and rehabilitation protocols.
Other Potential Applications
Beyond epilepsy, depression, and stroke recovery, ongoing research is exploring the potential of VNS in treating other conditions. One such area of interest is Alzheimer’s disease, where VNS has been shown to stimulate hippocampal neurogenesis and potentially enhance cognitive function through brain stimulation. Another area of interest is the treatment of headaches, with recent studies indicating that non-invasive vagus nerve stimulation (nVNS) has the potential to significantly reduce migraine or headache days.
These emerging applications underscore the versatility and potential of VNS in addressing a wide range of medical conditions. As research continues to uncover new possibilities, it is likely that the scope of VNS applications will continue to expand, offering hope to countless individuals affected by various medical conditions.
Risks and Side Effects of VNS
Like any medical intervention, VNS therapy carries some risks and side effects, particularly with invasive methods. Implantation of the vagus nerve stimulator may cause:
Voice alteration
Cough
Dyspnea
Dysphagia
Neck pain or paresthesias
It is essential to be aware of these potential side effects, especially when using anti inflammatory medications, and to work closely with healthcare providers to manage them effectively.
In addition to the side effects associated with the therapy itself, there are also risks associated with the surgical implantation of the VNS device. These risks are rare but similar to those of other surgical procedures. Patients should discuss these risks with their healthcare providers and weigh the potential benefits against any potential complications before deciding to undergo VNS therapy.
Surgical Risks
The surgical risks associated with implanting a VNS device are uncommon but similar to those of other surgical procedures. Potential complications of the procedure may include wound infection. Hoarseness, which may be temporary or permanent left vocal cord paralysis, is a risk in approximately 1% of patients..
The risk of infection associated with Vagus Nerve Stimulation surgery is relatively low, estimated to be around 2%. Allergic reactions to the implanted VNS device are infrequent but may occur.
Discussing these risks with your healthcare provider and considering them in your decision-making process about whether to pursue VNS therapy is vital.
Post-Surgery Side Effects
After undergoing VNS surgery, patients may experience the following side effects:
Voice changes
Hoarseness
Throat pain
Cough
Headaches
Shortness of breath
Difficulty swallowing
However, these side effects can often be managed by adjusting the intensity of the electrical impulses as needed.
If the side effects are not tolerable, the device can be temporarily or permanently adjusted or turned off. Working closely with healthcare providers, patients can find a balance between managing side effects and experiencing the benefits of VNS therapy.
Preparing for VNS Therapy
Prior to starting VNS therapy, discussing options with healthcare providers, understanding the procedure, and adhering to pre-surgery instructions are paramount. This preparation stage ensures that patients are in the best possible position to benefit from VNS therapy and manage any potential risks or side effects.
In addition to discussing the procedure with healthcare providers, patients should also familiarize themselves with the implantation process and what to expect during recovery. This may involve adjusting medications, adhering to fasting protocols, and undergoing a physical exam to ensure optimal health prior to surgery.
Pre-Surgery Preparations
Before the VNS implantation procedure, patients should make any necessary medication adjustments based on their healthcare provider’s guidance. Fasting for 6 hours for easily digested solids and 2 hours for clear liquids is typically recommended.
A physical exam, which may involve blood tests and other medical tests, is usually conducted to ensure the patient is in optimal health and is an eligible candidate for the surgery.
The VNS Implantation Procedure
The VNS implantation procedure involves:
Making two incisions, one on the left side of the neck and the other on the upper left chest.
Carefully wrapping the coil electrodes at the end of the lead wire around the left vagus nerve through the neck incision.
Guiding the lead wire down to the chest and securely connecting it to a battery.
The device is activated at the initial setting for a period of 30-90 seconds to test its capability to stimulate the vagus nerve, and the surgeon evaluates the system.
The procedure is generally conducted under general anesthesia.
Results and Effectiveness of VNS
While VNS is not a definitive treatment for medical conditions, it has demonstrated encouraging outcomes in treating various conditions such as epilepsy, treatment-resistant depression, and stroke recovery. The effectiveness of VNS varies depending on the specific condition and the individual patient, but many patients have experienced significant improvements in their conditions as a result of VNS therapy.
As research continues to uncover new possibilities for VNS, it is likely that the scope of VNS applications will continue to expand, offering hope to countless individuals affected by various medical conditions. It is important to remember, however, that VNS may not work for everyone and is not a cure. The next sections will provide a more detailed examination of the specific outcomes and effectiveness of VNS in treating a variety of medical conditions.
Seizure Reduction in Epilepsy
VNS has been effective in reducing seizures in patients with epilepsy who do not respond to medications. Studies have indicated that VNS therapy can lead to a seizure frequency reduction of ≥ 50% in some patients post-implantation, with up to 50% fewer seizures and less intense seizures.
However, keep in mind that not all patients achieve a seizure-free status. Approximately 60% of epilepsy patients typically respond to Vagus Nerve Stimulation with a ≥50% reduction in seizure frequency.
The effectiveness of VNS in treating epilepsy depends on the specific type of epilepsy and the individual patient, but it has shown promise in helping many patients achieve better seizure control.
Mood Improvement in Depression
For those dealing with treatment-resistant depression, VNS therapy has shown improvements in mood and quality of life. Patients who undergo VNS therapy for depression may experience improved mood and quality of life as a result of the treatment. Research has demonstrated significant mood improvement and efficacy in individuals with treatment-resistant depression.
Nevertheless, understand that the level of improvement with VNS therapy can vary among individuals suffering from treatment-resistant depression. Factors such as the severity of the condition, the presence of comorbid conditions, and the specific type of VNS therapy used can all influence the effectiveness of the treatment.
Stroke Rehabilitation
Stroke rehabilitation is a critical aspect of regaining function and independence following a stroke. VNS has been FDA-approved in combination with rehabilitation for hand and arm function recovery following an ischemic stroke. VNS rapidly activates key neuromodulators in the brain, promoting synaptic reorganization and enhancing plasticity in the motor cortex, leading to improved motor function and recovery after stroke.
Participants with moderate to severe arm impairment after ischemic stroke demonstrated clinically significant improvements in motor impairment and function with VNS therapy. VNS therapy paired with rehabilitation may lead to a greater improvement in distal upper extremity function in comparison to rehabilitation alone. This highlights the potential benefits of incorporating VNS into stroke recovery and rehabilitation protocols.
Patient Experiences with VNS
Patient experiences with VNS vary, with some reporting:
significant improvements in their conditions
a significant reduction in seizure activity following VNS Therapy
significant mood improvement and efficacy in individuals with treatment-resistant depression
However, others may not see the same level of success.
Bear in mind that the effectiveness of VNS can differ based on the specific medical condition and the individual patient’s circumstances. Some patients may experience life-changing improvements in their conditions, while others may not see the same level of success. Nevertheless, VNS therapy offers hope to countless individuals affected by various medical conditions.
See Patient Stories – VNS Therapy Epilepsy
Summary
Vagus Nerve Stimulation (VNS) is an innovative therapy that has shown promising results in treating various medical conditions, including epilepsy, treatment-resistant depression, and stroke recovery. While it may not work for everyone and is not a cure, VNS therapy offers hope to countless individuals affected by these conditions. As research continues to explore new applications and refine existing techniques, the potential benefits of VNS are likely to grow, providing hope and improved quality of life for many patients.
Frequently Asked Questions
How do I stimulate the vagus nerve?
To stimulate the vagus nerve, you can try plunging your face into ice water baths, engaging in neck and ear massage, doing eye exercises, deep breathing, humming or singing, listening to calming music, gargling with water, having a foot massage, and immersing your forehead in cold water.
What are the symptoms of an irritated vagus nerve?
Common symptoms of an irritated vagus nerve include abdominal pain and bloating, acid reflux, changes in heart rate, blood pressure or blood sugar, difficulty swallowing or loss of gag reflex, dizziness or fainting, and hoarseness, wheezing or loss of voice.
Where is the pressure point for the vagus nerve?
HT 7, located on the wrist, and the fleshy cartilage in the front of the ear are both effective pressure points for stimulating the vagus nerve, helping to reduce anxiety and promote relaxation.
What is the main purpose of Vagus Nerve Stimulation (VNS) therapy?
VNS therapy is a therapeutic technique that uses electrical impulses to stimulate the vagus nerve to treat conditions like epilepsy, depression, and stroke recovery, providing a safe and effective treatment option for those who don’t respond to other forms of therapy.
How does invasive VNS differ from non-invasive VNS?
Invasive VNS involves the implantation of a device, while non-invasive VNS uses transcutaneous electrical stimulation to stimulate the vagus nerve, making them two distinct forms of therapy.