What are the health risks associated with obesity? Excess body weight predisposes individuals to a higher likelihood of developing life-altering conditions, such as heart disease, type 2 diabetes, and breathing issues. This article will guide you through the complexities of the danger of obesity, shedding light on the significant health threats and the actionable steps you can take to improve your health and reduce these risks.
Table of Contents
Key Takeaways
Obesity significantly increases the risk of various health conditions including type 2 diabetes, heart disease, respiratory problems, and certain cancers, making weight management crucial for reducing these risks.
Excess body fat not only affects physical health, leading to cardiovascular disease, diabetes, respiratory, liver, and kidney issues, but also impacts mental health, contributing to depression and low self-esteem.
Preventing and treating obesity requires a multifaceted approach including diet and exercise, medical interventions like bariatric surgery for severe cases, and societal support to promote healthy lifestyles and reduce weight stigma.
The Perils of Excess Body Fat: Understanding the Risks

The health risks associated with excess body fat manifest even when a person is just slightly overweight, increasing in severity as more weight is gained. Severe obesity correlates with a range of significant health issues, including:
type 2 diabetes
high blood pressure
heart disease
respiratory problems
The good news is that losing even a modest amount of weight—between 5% to 10% of body weight—can provide meaningful health benefits.
Understanding these risks is the first step towards effective obesity management. By recognizing how excess weight contributes to various health problems, individuals can take proactive measures to lose weight and improve their overall health.
Addressing obesity isn’t merely about achieving a healthy weight; it’s about reducing the risk factors that lead to chronic disease and enhancing quality of life through effective disease control.
Heart Disease and Stroke: The Weighty Connection
Excess weight is a significant risk factor for heart disease and stroke. Obesity contributes to cardiovascular risks by increasing the likelihood of high blood pressure and high cholesterol. The presence of these conditions increases the likelihood of developing coronary heart disease, stroke, and cardiovascular death. This elevates the overall risk to an individual’s health.
Furthermore, metabolic syndrome, a condition often associated with obesity, combines the following factors that exacerbate the risk of developing cardiovascular disease:
Increased blood pressure
High blood sugar
Excess body fat around the waist
Abnormal cholesterol levels
Losing weight can significantly reduce these risks, highlighting the importance of maintaining a healthy weight to protect heart health.
Diabetes: The Heavy Burden of Blood Sugar Imbalance
Being obese significantly increases the risk of developing type 2 diabetes. This is a well-established connection in medical research. Individuals affected by obesity are about six times more likely to develop high blood sugar, which can lead to type 2 diabetes. For women with a BMI of 35 or higher, the risk of developing diabetes is 93 times higher compared to those with lower BMIs. This stark statistic underscores the heavy burden that excess weight places on the body’s ability to regulate blood glucose levels.
Effective weight management and lifestyle changes are crucial for preventing diabetes and its associated health problems.
Respiratory Complications: When Weight Impairs Breathing
The link between obesity and respiratory complications is well-documented. Conditions like asthma and obstructive sleep apnea are closely associated with excess weight. Approximately one in five adults is affected by obstructive sleep apnea, a condition frequently linked to obesity. In fact, between 50% and 75% of individuals with obstructive sleep apnea are obese.
Moreover, obesity increases the risk of developing asthma by 50%. These respiratory issues can significantly impair quality of life, but the good news is that modest weight loss can help treat sleep apnea and improve lung health.
Unseen Dangers: Obesity’s Impact on Internal Systems
While the visible effects of obesity are concerning, the unseen dangers it poses to internal organs and systems are equally alarming. Obesity negatively affects internal organs, including the liver, kidneys, and other critical systems. For instance, nonalcoholic fatty liver disease (NAFLD) is closely linked to obesity and represents a significant health concern due to the potential for liver damage. Moreover, the increased adipocyte mass and heightened lipid levels associated with obesity contribute to the risk of developing cancers.
The inflammatory responses heightened by obesity not only have immediate health impacts but can also accelerate cancer progression. Understanding these internal dangers is crucial for recognizing the full scope of obesity’s impact on health. By addressing these issues through weight loss and healthier lifestyle choices, individuals can mitigate these risks and improve their overall well-being.
Liver at Risk: Tackling Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease (NAFLD) is a major concern for individuals with obesity. A high prevalence of NAFLD is seen in those who are overweight or obese, with estimates indicating that 80% to 90% may suffer from liver diseases like NAFLD and non-alcoholic steatohepatitis (NASH). If not addressed, NAFLD can escalate to more severe conditions such as fibrosis, cirrhosis, and potentially liver failure.
Addressing obesity through lifestyle intervention and treating obesity is vital to prevent these serious liver complications.
Kidneys Under Pressure: Obesity’s Role in Chronic Kidney Disease
Excess weight significantly increases the risk of chronic kidney disease (CKD). The additional workload placed on the kidneys and the increased risk of high blood pressure and diabetes due to obesity contribute to kidney damage. It’s essential to understand that managing body weight effectively can help reduce the strain on the kidneys and lower the risk of CKD.
Monitoring BMI, a critical measure used to categorize weight status, and maintaining it within a healthy range is crucial for kidney health.
Metabolic Mayhem: Consequences of Metabolic Syndrome
Metabolic syndrome is a cluster of conditions that frequently occur together and are linked with an increased risk of heart disease and other health problems. These conditions include:
Increased blood pressure
High blood sugar
Excess body fat around the waist
Abnormal cholesterol levels
One of the hallmarks of metabolic syndrome in individuals with severe obesity is insulin resistance, which can further exacerbate metabolic complications.
Addressing these interconnected issues through weight loss and lifestyle changes is essential to mitigate the health risks associated with metabolic syndrome.
The Psychological Toll: Mental Health and Obesity
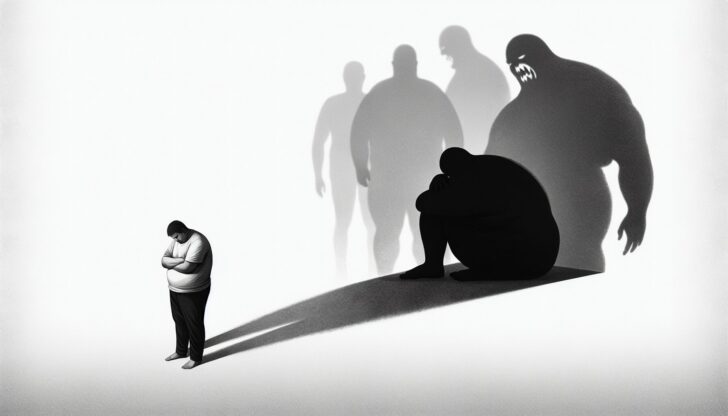
Obesity doesn’t just affect the body; it takes a significant toll on the mind as well. Individuals with obesity are at a 55% increased risk of developing depression over their lifetime, and those with depression have a 58% higher risk of becoming obese. The psychological impact of obesity is profound, often leading to reduced self-esteem, fewer employment opportunities, and substandard healthcare due to weight bias and discrimination. Experiencing weight stigma can be a daily occurrence for individuals with obesity, leading to psychological distress and harmful behaviors such as binge eating and avoiding exercise.
Coping with weight stigma involves various strategies, with reappraisal coping being adaptive and associated with better well-being, while disengagement coping is maladaptive and correlates with poorer mental health. Addressing these psychological challenges is just as important as tackling the physical health risks of obesity. By fostering a supportive environment and promoting mental health alongside physical health, individuals can achieve a holistic approach to weight management.
Body Image and Self-Esteem: Rebuilding Confidence
Individuals with obesity often struggle with low self-esteem due to societal standards and personal dissatisfaction with their body image. The stigma and prejudice associated with weight can exacerbate feelings of rejection and social isolation.
Achieving a healthy weight has been linked with improvements in body image and the perception of one’s attractiveness and physical capabilities. Successful weight management can lead to a sense of accomplishment, fostering increased confidence and better mental health.
Developing realistic goals, engaging in positive self-talk, and practicing self-compassion are essential steps for rebuilding body confidence and self-esteem.
Coping with Stigma: Addressing Weight-Related Bias
Weight-related stigma stems from societal stereotypes that unfairly label individuals with obesity as unattractive, lazy, and undisciplined. This negative bias can significantly impact a person’s body image, leading to feelings of embarrassment and dissatisfaction with one’s appearance. Coping with weight bias often involves:
Seeking social support
Confronting those who discriminate
Engaging in social activism
Employing disengagement tactics to avoid stigma.
Addressing these biases and fostering a more inclusive environment is crucial for the mental health and well-being of individuals with obesity.
Mobility and Musculoskeletal Challenges

Excess weight places significant mechanical and metabolic strain on bones, muscles, and joints, increasing the risk of musculoskeletal disorders and disabilities. Obesity is associated with a higher incidence of joint problems, leading to an array of orthopedic health issues, including osteoarthritis. Additionally, the inflammation of tendons, known as tendonitis, can result from excess body weight as tendons around the joints struggle with the increased load. These issues underline the importance of maintaining a healthy weight to preserve mobility and joint health.
Furthermore, individuals who are obese are more likely to undergo knee replacement surgery due to the additional pressure placed on their joints. Addressing obesity through weight loss can significantly reduce the risk of these musculoskeletal challenges and improve overall quality of life.
Osteoarthritis: The Weight-Bearing Struggle
Excess body fat can lead to musculoskeletal disorders such as osteoarthritis. For every pound of body weight, there is an equivalent of four to six pounds of pressure exerted on each knee joint, exacerbating the risk of osteoarthritis. Even being 10 pounds overweight can add between 15 to 50 pounds of additional pressure on the knees, raising the likelihood of developing osteoarthritis or worsening existing conditions.
Weight loss can significantly reduce arthritis pain, with a 10% reduction in body weight potentially halving the pain. These improvements highlight the importance of weight management in mitigating joint problems.
The Link Between Body Weight and Back Pain
Excessive body weight adds mechanical stress to the spine, increasing the risk for back pain. Systemic inflammation is another contributing factor to back pain in individuals with obesity.
Engaging in physical activity is essential for managing obesity and can help mitigate the effects of back pain by strengthening the muscles supporting the spine. By addressing these issues through weight loss and regular exercise, individuals can improve their spinal health and reduce back pain.
Reproductive and Sexual Health Complications
Obesity can have profound effects on reproductive and sexual health. In women, obesity can disrupt hormone balance, leading to:
Menstrual irregularities
Fertility issues
Increased risk of miscarriage
Gestational diabetes
Preeclampsia
Complications during labor and delivery
These are all associated with obesity.
For men, increased BMI is linked to a higher likelihood of experiencing erectile dysfunction, which may improve with weight loss. Addressing these issues is crucial for improving reproductive and sexual health outcomes in individuals with obesity.
Understanding the full scope of these complications can help individuals take proactive steps towards weight management, improving not only their reproductive health but also their overall well-being.
Fertility Concerns: How Obesity Affects Conception
Women with a Body Mass Index (BMI) above 27 are significantly more likely to be anovulatory, tripling the difficulty in conceiving. In women who are able to ovulate, having a higher BMI is linked to poorer egg quality and a reduced likelihood of achieving pregnancy within one year. Obesity-related changes in hormone levels, such as decreased adiponectin and increased leptin, have been implicated in the development of infertility.
Addressing obesity through lifestyle changes and weight management can improve fertility outcomes and enhance reproductive health.
Intimacy Issues: Weight’s Effect on Sexual Function
Obesity is linked to sexual dysfunction in both men and women and can negatively impact sexual health. Obese men are more likely to suffer from erectile dysfunction and may have lower testosterone levels due to excess body fat. Overweight women have a higher risk of infertility and may experience reductions in sexual desire and satisfaction.
The psychological burden of obesity, including low self-esteem and body image issues, can contribute to intimacy problems and sexual dissatisfaction. Addressing these issues through weight loss and healthy lifestyle choices can improve sexual function and overall quality of life.
Cancer Risk and Obesity: A Growing Concern
Being overweight or obese is the second most significant risk factor for developing a wide range of cancers. In addition to obesity, other risk factors are also linked to an increased risk of several types of cancer, including:
Breast cancer
Colon cancer
Endometrial cancer
Kidney cancer
Esophageal cancer
Gallbladder cancer
Ovarian cancer
Pancreatic cancer
This association underscores the importance of weight management in cancer prevention. By adopting healthier lifestyle habits and striving for a healthy weight, individuals can significantly reduce their risk of developing these cancers.
The connection between obesity and cancer emphasizes the need for comprehensive prevention strategies. These strategies should focus on promoting weight management through diet, physical activity, and other health-promoting behaviors. Understanding the obesity-cancer link can motivate individuals to take proactive steps towards a healthier lifestyle, ultimately reducing their cancer risk.
Understanding the Obesity-Cancer Connection
Excess body fat actively promotes cancer risk by sending damaging cellular signals and contributing to inflammation. Abdominal obesity and weight gain during adulthood are linked with several cancers, including breast, colon, and rectum, endometrium, esophagus, kidney, ovary, and pancreas. Cancer cells can thrive on lipids originating from adipose tissue, with obesity increasing the supply through mechanisms such as de novo lipogenesis or lipid transfer from adjacent fat cells.
Additionally, white adipose tissue-derived mesenchymal stem cells, which are more abundant in obesity, can facilitate tumor growth by integrating into tumor blood vessels or turning into adipocytes that support the tumor. These insights highlight the importance of understanding and addressing the obesity-cancer connection.
Navigating the Path to a Healthier Life: Prevention and Treatment
Preventing obesity requires the collective effort of various societal sectors, including governments, schools, businesses, communities, and families, to ensure healthy choices are easily accessible. Effective obesity prevention entails policy and environmental efforts aimed at promoting healthier eating, encouraging physical activity, reducing sedentary screen time, and supporting adequate sleep and reduced stress. Settings like family homes, schools, and healthcare organizations can adopt comprehensive recommendations that enhance their environments to foster healthier lifestyle habits.
By creating supportive environments and fostering healthy behaviors, we can collectively combat the obesity epidemic. From policy changes to individual lifestyle interventions, every effort counts towards building a healthier future.
Lifestyle Intervention: Diet and Physical Activity
Incorporating a healthier diet and engaging in regular physical activity are key behavioral strategies for preventing obesity. Incorporating more plant-based foods, fruits, vegetables, and whole grains while limiting salt, sugar, and unhealthy fats can contribute to a healthier diet and weight management.
Preventing further weight gain or maintaining weight loss requires at least 150 minutes a week of moderate-intensity physical activity. These lifestyle interventions not only help in losing weight but also in maintaining a healthy weight and preventing obesity-related diseases.
Medical Approaches: When to Consider Weight Loss Surgery
For individuals with severe obesity, medical approaches such as bariatric surgery and endoscopic procedures can be considered. Some options include:
Gastric bypass: This procedure limits food intake and nutrient absorption to promote weight loss.
Sleeve gastrectomy: This procedure also limits food intake by removing a portion of the stomach.
Intragastric balloons: This is a less invasive procedure where a balloon is placed in the stomach to reduce its capacity.
Endoscopic sleeve gastroplasty: This procedure uses sutures to reduce the size of the stomach.
These medical interventions offer a way to address severe obesity and promote weight loss.
These medical treatments can be effective for those who have not achieved significant weight loss through lifestyle changes alone.
Learn more, visti Thinking about weight-loss surgery? 4 things to consider.
Summary
In summary, obesity is a complex health issue with far-reaching consequences. It increases the risk of numerous health conditions, including heart disease, diabetes, respiratory issues, liver and kidney diseases, metabolic syndrome, mental health problems, musculoskeletal challenges, reproductive and sexual health complications, and cancer. Understanding these risks is crucial for effective obesity management. By adopting healthier lifestyle habits, seeking medical interventions when necessary, and creating supportive environments, individuals can achieve and maintain a healthy weight, reducing their risk of obesity-related diseases and improving their overall quality of life. Let’s commit to making informed choices and supporting each other on the journey to better health.
Frequently Asked Questions
How does obesity increase the risk of heart disease?
Obesity increases the risk of heart disease by raising blood pressure and cholesterol levels, which in turn can lead to coronary heart disease and stroke.
What is the relationship between obesity and type 2 diabetes?
Obesity is a significant risk factor for type 2 diabetes, as individuals affected by obesity are about six times more likely to develop high blood sugar, leading to type 2 diabetes.
How does obesity affect respiratory health?
Obesity can have a significant impact on respiratory health, increasing the risk of conditions such as asthma and obstructive sleep apnea. This connection highlights the importance of managing weight for overall respiratory well-being.
What are the psychological impacts of obesity?
Obesity can significantly increase the risk of developing depression and result in weight-related stigma, which can lead to lower self-esteem and psychological distress. It’s important to address these impacts to support overall well-being.
When should weight loss surgery be considered?
Weight loss surgery should be considered for individuals with severe obesity who have not achieved significant weight loss through lifestyle changes alone. It can include bariatric surgery and endoscopic procedures.