As of 2023, 41.9% of American adults are affected by obesity—a concerning statistic that mirrors a deeper public health challenge. Through this exploration of the America obesity rate, we’ll uncover the intricacies of the issue, its wide-reaching implications, and initiatives to curtail its impact.
Table of Contents
Key Takeaways
Adult obesity rates in America have reached 41.9% as of 2023, presenting a significant public health challenge that necessitates targeted interventions across all age groups and demographics.
Childhood and adolescent obesity are also growing concerns, with 19.7% of U.S. children and adolescents categorized as obese, indicating the need for early intervention and prevention strategies to address obesity at a young age.
Obesity in America is characterized by disparities across race, income, and geography; effective public health strategies and interventions must consider these differences to tackle obesity and reduce its associated medical and economic burdens.
The Current State of Adult Obesity in America
Adult obesity rates in America have reached alarming levels, with 41.9 percent of U.S. adults classified as obese as of 2023. This reflects a significant public health challenge, as obesity is linked to numerous health consequences and chronic diseases. Obesity prevalence varies among age groups. 35.7% of adults aged 20-39, 42.8% of those aged 40-59, and 41.0% of adults aged 60 and over are affected by obesity. These variations highlight the need for targeted interventions across all age groups to address the growing obesity epidemic.
The rise in obesity rates has been consistent over the past few decades, signaling a concerning trend for America’s health. As adult obesity rates persist in their upward trend, gaining insight into the contributing factors and formulating impactful prevention and management strategies is imperative.
Unpacking the Numbers: Prevalence of Obesity Among Adults
Interpreting the prevalence of obesity among adults requires a careful examination of the data. According to the CDC, the age-adjusted prevalence rate for obesity in American adults was 39.7% in 2017, with men at 37.9% and women at 41.1%. These figures highlight the significant gender disparities in obesity rates, which must be considered when developing targeted interventions. However, recognizing potential biases in self-reported surveys is important, as they can distort the accuracy of obesity statistics due to individuals’ tendencies to overestimate their height and underestimate their weight.
Despite these challenges, accurate data interpretation remains essential for addressing obesity effectively. Gaining a clear understanding of obesity prevalence allows public health officials and policymakers to optimally allocate resources and design interventions targeting the root causes of this epidemic. Accurate obesity reports are vital for informing strategies to combat obesity and promote healthier lifestyles among the population.
Analyzing Trends Over Time
Obesity rates have been on a steady incline over the past three decades, reflecting a general upward trend in adult obesity. Since the first State of Obesity report in 2004, the national adult obesity rate has increased by 37 percent. This trend underscores the need for continued efforts to address the factors contributing to obesity and to promote healthier behaviors among the population.
Variations in obesity rates across different races and ethnic groups further complicate the landscape of obesity trends. For instance, projections estimate that by 2030, 86.3% of adults will be overweight or obese, and 51.1% will be obese. These alarming projections highlight the urgency of implementing effective interventions to reverse the upward trajectory of obesity rates and improve america’s health.
Childhood and Adolescent Obesity: A Growing Concern
Childhood and adolescent obesity have emerged as significant public health concerns, with the prevalence of obesity among U.S. children and adolescents aged 2-19 years reported at 19.7% from 2017 to March 2020. This high prevalence underscores the importance of early intervention and prevention strategies to combat obesity from a young age. Obesity in children and adolescents is determined by a body mass index (BMI) at or above the 95th percentile on the sex-specific BMI-for-age CDC Growth Charts. This helps healthcare professionals in assessing the weight status of individuals in this age group.
Obesity rates among youth have remained stable since 2003-2004, but both adults and youth have experienced significant increases in obesity from 1999 to 2013-2014. This trend indicates that the obesity epidemic affects individuals across all age groups, necessitating comprehensive approaches to address this issue and promote healthier lifestyles among children and adolescents.
Spotlight on Child Obesity
The prevalence of child obesity has seen a dramatic rise over the past few decades. Between 1980 and 2008, there was a significant increase in the prevalence of obesity in children aged 6 to 11 years, almost tripling from 6.5% to 19.6%. This historical rise highlights the urgent need for interventions to reverse the trend of childhood obesity. Ensuring that children have access to healthy foods and opportunities to be physically active is central to addressing this issue.
Out-of-school time (OST) programs play a crucial role in promoting healthy lifestyles among children. These programs engage millions of children in activities that support physical activity and healthy eating habits beyond the school day. Providing nutritious afterschool snacks and meals is an essential component of these programs, reinforcing healthy eating patterns among children. A focus on cultivating healthy environments can aid in reducing child obesity prevalence, promoting improved health outcomes for future generations.
Adolescent Obesity: Challenges and Consequences
Adolescent obesity presents unique challenges and long-term health consequences. The prevalence of obesity in teenagers increased from 5% in 1980 to 18.1% in 2008, more than tripling over the 28-year period. This significant increase highlights the need for targeted interventions to address the factors contributing to adolescent obesity. Overweight adolescents have a 70 percent chance of becoming overweight or obese adults, indicating significant long-term health risks.
The health consequences of adolescent obesity are far-reaching, including an increased risk of developing chronic diseases such as diabetes and cardiovascular conditions later in life. Early intervention is crucial to mitigate these risks and promote healthier lifestyles among adolescents. Addressing adolescent obesity’s root causes and implementing impactful prevention strategies can assist in reducing obesity prevalence and enhancing young adults’ overall health.
Disparities in Obesity: Race, Income, and Geography
Obesity prevalence in America is marked by significant disparities across different races, incomes, and geographies. African Americans and Latinos experience higher rates of obesity compared to Whites, while Asians have lower rates. These disparities highlight the need for targeted interventions that consider the unique challenges faced by different population groups.
Socioeconomic, racial, and ethnic disparities in obesity prevalence and trends have been documented across the United States. Understanding these disparities is essential for developing effective strategies to address obesity and promote health equity. Examining the variations in obesity rates across diverse demographic groups enables the tailoring of interventions to meet each community’s unique needs.
Racial and Ethnic Variations in Obesity Rates
Racial and ethnic variations in obesity rates are stark, with the highest rates observed among Black adults (49.9%) and Latino adults (45.6%). African American women have the highest prevalence of obesity, while Asian American women have the lowest among racial groups. In California, ethnic disparities in obesity are pronounced, with African Americans showing a rate three times that of Asians.
These significant differences underscore the need for culturally sensitive interventions to address obesity among different racial and ethnic groups. Understanding the distinct factors contributing to obesity in these populations facilitates the development of targeted strategies to foster healthier lifestyles and lessen health disparities.
The Impact of Socioeconomic Status on Obesity
Socioeconomic status plays a crucial role in obesity prevalence, with lower-income individuals experiencing higher rates of obesity. The prevalence of obesity is lower among adults in the highest income group (31.2%) compared to those earning between 130% to 350% above the poverty line (40.8%) and those at or below 130% of the poverty line (39.0%). Residents of rural areas also demonstrate higher obesity rates than their urban and suburban counterparts.
These disparities highlight the need for targeted interventions that address the societal and environmental factors contributing to obesity. Some strategies to consider include:
Enhancing access to healthy foods in lower-income and rural communities
Increasing physical activity opportunities in these areas
Implementing nutrition education programs to promote healthy eating habits
Creating safe and accessible spaces for physical activity, such as parks and community centers
By focusing on these interventions and implementing effective disease control measures, we can contribute to a reduction in obesity prevalence, helping people to lose weight and achieve improved health outcomes for all.
Mapping Obesity: State-by-State Analysis
Obesity rates vary significantly across different states, showcasing geographic disparities in obesity prevalence. In 2022, 22 states had an adult obesity rate at or above 35 percent, marking an increase from 19 states the year before. West Virginia, Louisiana, Oklahoma, and Mississippi have the highest rates of adult obesity, while the District of Columbia, Colorado, and Hawaii have the lowest.
These geographic disparities highlight the importance of state-specific interventions to address obesity. Understanding the unique challenges each state faces allows policymakers to devise targeted strategies, promoting healthier behaviors and reducing obesity rates nationwide.
Chronic Diseases and Obesity: The Health Consequences
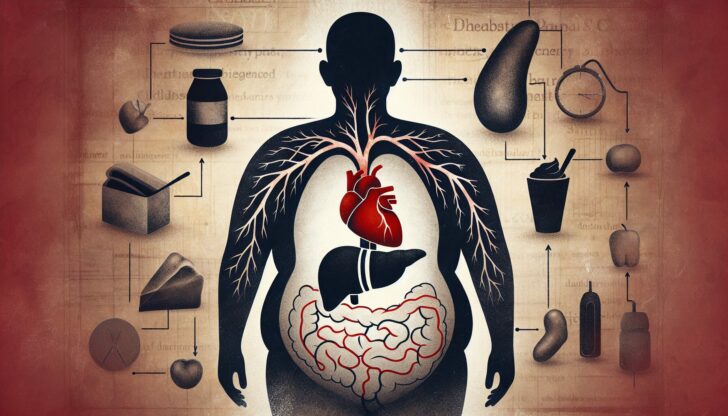
Obesity is characterized by an increase in the size and amount of fat cells in the body, leading to a higher body mass index (BMI) and weight gain. As an independent risk factor, obesity contributes to various chronic diseases, including cardiovascular diseases, diabetes, and certain cancers. A reduction of 5-10% in body weight can lead to a substantial decrease in the risk of chronic diseases for individuals with obesity.
Certain risk factors, such as age, arthritis, and diabetes medication intake, are consistent across all ethnic groups in contributing to higher BMI and obesity. Targeted interventions addressing these risk factors can contribute to a reduction in obesity prevalence and enhanced overall health outcomes.
Heart Disease, High Blood Pressure, and Obesity
Obesity is considered a cause of heart disease. The increase in adipose tissue associated with obesity results in the secretion of adipokines, leading to hypertension and other cardiovascular risk factors. The augmented stroke volume and cardiac output due to excess adiposity can result in heart structure alterations like left ventricular hypertrophy.
These physiological changes lead to cardiomyopathy and heart failure through diastolic dysfunction and are associated with increased atherosclerotic plaque burden and inflammation in plaques. Addressing obesity contributes to a reduced risk of heart disease and improved cardiovascular health.
Diabetes and Obesity: A Dangerous Connection
Obesity creates a pro-inflammatory state in the body that can lead to insulin resistance. Adipokine imbalance, which occurs due to excess fat tissue, is a contributor to the inflammatory state associated with obesity. Insulin resistance, often exacerbated by obesity, is a key determinant in the development of metabolic syndrome and type 2 diabetes.
Over 80% of individuals with coronary heart disease are overweight or obese, linking obesity with increased risk factors for type 2 diabetes, such as high blood pressure and insulin resistance. Addressing obesity is key to curtailing the prevalence of diabetes and enhancing overall health outcomes.
Addressing Obesity: Interventions and Public Health Strategies

Effective interventions and public health strategies are essential for addressing obesity. Workplace initiatives play a critical role in obesity prevention and management strategies. According to the World Health Organization, comprehensive programs in the workplace aimed at health improvement can lead to more positive health behaviors among employees.
Implementing effective obesity prevention strategies within the workplace can lead to a decrease in overall obesity rates among employees. These strategies can include promoting physical activity, healthy eating, and making environmental modifications to support healthier behaviors.
Promoting Physical Activity and Healthy Foods
Promoting physical activity and healthy food choices is crucial for combating obesity. Health behaviors associated with diet and physical activity, often influenced by socioeconomic status, contribute to disparities in obesity rates. Moderate physical activity combined with weight loss efforts can lead to a substantial reduction in type 2 diabetes incidence among at-risk individuals.
Efforts to combat obesity often include strategies that promote increased access to opportunities for physical activity and make healthy eating options more accessible. Adoption of voluntary healthy eating and physical activity standards in out-of-school time programs enhances the promotion of a healthy lifestyle.
Occupational and Environmental Medicine Approaches
Occupational and environmental medicine approaches play a vital role in addressing obesity by focusing on the workplace. Recognizing the significant amount of time adults spend at work and the diverse population present, workplaces serve as key settings for implementing obesity control programs. Environmental factors within the workplace, such as easy access to high-calorie foods and limited opportunities for physical activity, can influence obesity.
Comprehensive worksite interventions that incorporate environmental modifications alongside targeted strategies for individuals have shown promise in weight management and control. Successful worksite health interventions have led to enhanced physical activity options and better nutrition information availability, contributing to healthier workplace environments.
Policy Measures and Their Effectiveness
Policy measures are critical in addressing obesity on a broader scale. Taxes on sugary drinks, for example, are a strategy implemented to control obesity issues. These taxes aim to reduce the consumption of high-calorie beverages and promote healthier choices. In mid-2006, the American Beverage Association committed to a voluntary ban on the sale of all high-calorie drinks in schools to address obesity.
Calorie labeling policies require chain restaurants to post calorie information on menus and provide additional nutrition information upon request. The introduction of proper labeling has led to consumers purchasing fewer unhealthy food products and more healthier options. These policy measures have proven effective in promoting healthier behaviors and reducing obesity rates.
The Economic Burden of Obesity
The economic burden of obesity is substantial, with obesity in the US resulting in over $200 billion in medical costs annually. The total medical costs attributed to obesity among U.S. adults in 2016 was estimated at $260.6 billion. These staggering figures highlight the significant impact of obesity on healthcare systems and economies.
Projected healthcare costs related to obesity by 2030 could reach up to $956.9 billion. The total costs of obesity are estimated to range from 0.05% to 2.24% of a country’s gross domestic product (GDP). Addressing the economic burden of obesity requires comprehensive strategies that include prevention, management, and policy measures to reduce the prevalence of obesity and its associated costs.
Calculating the Costs: Direct and Indirect Expenses
Calculating the costs associated with obesity involves both direct and indirect expenses. Adults with obesity in the U.S. face average annual medical care costs that are $2,505 higher compared to those with normal weight. The medical costs for children with obesity were on average $116 higher per person per year compared to children of a healthy weight, and $310 higher for those with severe obesity.
Indirect costs of obesity include:
Reduced work productivity due to absenteeism and presenteeism
Increased rates of premature mortality and disability benefit payments
Loss of Quality Adjusted Life Years (QALYs)
These costs highlight the broader economic impact of obesity beyond just medical expenses.
Healthcare Access and Obesity
Healthcare access plays a crucial role in addressing obesity and its associated costs. Medicare and Medicaid provide health coverage to 40% of individuals with obesity and to 46% of those with obesity-related comorbidities and complications. This coverage is essential for ensuring that individuals with obesity receive the necessary medical care and support for managing their condition.
Improving healthcare access can help reduce health disparities and promote better health outcomes for individuals with obesity. Increasing access to healthcare services and interventions can aid in mitigating the economic burden of obesity and enhancing America’s health.
Body Mass Index (BMI): Understanding the Metric
Body Mass Index (BMI) is a widely used tool for estimating and screening for overweight and obesity in adults and children. BMI is a measure of body fat based on height and weight. It is calculated by dividing weight in kilograms by the square of height in meters. It is utilized as a simple and cost-effective screening method for classifying individuals into various weight categories, such as:
Underweight
Healthy weight
Overweight
Obesity
While BMI is a useful metric, it has limitations. BMI may not accurately reflect an individual’s body fat percentage or distribution, nor does it account for factors such as muscle mass, bone density, and overall body composition. Despite these limitations, BMI remains a valuable tool for public health officials and healthcare providers in assessing obesity and developing targeted interventions.
How BMI Is Calculated and Used
BMI is calculated by dividing an individual’s weight in kilograms by their height in meters squared. This calculation provides a numerical value that is used to classify individuals into standard weight status categories, which apply to both men and women of all ages and body types.
These categories help healthcare providers assess the risk of obesity-related health conditions and determine appropriate interventions. Understanding how BMI is calculated and used enables individuals to better interpret their weight status and take proactive steps towards achieving a healthy weight.
Critique of BMI: Is It a Reliable Indicator?
While BMI is intended as a straightforward metric for estimating the amount of body fat a person carries, it is not without its flaws. Although BMI has a moderate correlation with the amount of body fat, it is not a direct measure of body fatness. Factors such as muscle mass, bone density, and overall body composition can influence BMI, potentially leading to misclassification of individuals’ weight status.
Given these limitations, it is important to consider other measures and indicators, such as health statistics, when assessing an individual’s health and risk of obesity-related conditions. Using a combination of metrics allows healthcare providers to gain a comprehensive understanding of an individual’s health, enabling them to tailor interventions accordingly.
Learn more, visit Obesity Statistics And Facts In 2024 – Health.
Summary
In summary, obesity in America is a complex and multifaceted issue that requires a comprehensive approach to address. From the rising adult obesity rates to the growing concern of childhood and adolescent obesity, it is clear that targeted interventions and public health strategies are essential for combating this epidemic. Disparities in obesity prevalence across different races, incomes, and geographies further highlight the need for tailored approaches to address the unique challenges faced by diverse communities.
The health consequences of obesity, including its link to chronic diseases like heart disease and diabetes, underscore the urgency of addressing this issue. By promoting physical activity, healthy eating, and implementing effective policy measures, we can reduce the prevalence of obesity and improve overall health outcomes. Additionally, understanding the economic burden of obesity and improving healthcare access are crucial for mitigating the impact of obesity on healthcare systems and economies.
As we move forward, it is essential to continue developing and implementing comprehensive strategies to address obesity and promote healthier lifestyles. By working together, we can create a healthier future for all individuals and communities.
Frequently Asked Questions
What is the current state of adult obesity in America?
The current state of adult obesity in America is concerning, with 41.9 percent of U.S. adults being affected. Obesity prevalence varies across different age groups, with rates of 35.7% in adults aged 20-39, 42.8% among adults aged 40-59, and 41.0% among adults aged 60 and over.
How is childhood obesity defined?
Childhood obesity is defined as a body mass index (BMI) at or above the 95th percentile on the CDC Growth Charts.
What are the economic costs associated with obesity?
The economic costs associated with obesity are substantial, with estimated annual medical costs in the US exceeding $200 billion. This is a significant financial burden on the healthcare system.
How is BMI calculated and used?
BMI is calculated by dividing your weight in kilograms by your height in meters squared. It is used to determine your weight category, such as underweight, healthy weight, overweight, or obesity.
What are some effective policy measures to address obesity?
To address obesity, effective policy measures include implementing taxes on sugary drinks, enforcing voluntary bans on high-calorie drinks in schools, and requiring chain restaurants to provide calorie information on menus. These measures can help promote healthier choices and combat the obesity epidemic.









