Did you know that anticoagulant medications play a crucial role in preventing the formation of dangerous blood clots for millions of people worldwide? These life-saving drugs have vastly improved the quality of life for patients at risk of stroke, heart attack, and other clot-related issues. However, understanding the different types of anticoagulants, their uses, and potential side effects is vital to ensure safe and effective treatment. Dive into our comprehensive guide and discover everything you need to know about anticoagulants.
Table of Contents
Key Takeaways
Anticoagulant medicines inhibit the clotting process to reduce risk of stroke or heart attack.
Various types, such as DOACs and warfarin, require careful monitoring for potential side effects & interactions.
Patient resources are available to help manage anticoagulation therapy effectively.
Understanding Anticoagulants: How They Work
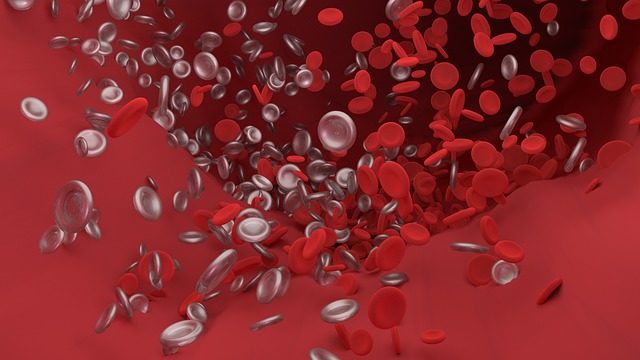
Anticoagulant medicines, also known as blood thinners, work by inhibiting the coagulation process, thus preventing the formation of blood clots. They target different stages of the blood clotting process and come in various types, including direct oral anticoagulants (DOACs), direct thrombin inhibitors, vitamin K antagonists, and heparin. Each type has its unique mechanism of action, which determines their appropriateness for specific medical conditions and individual patient needs.
To make informed decisions about your treatment plan, it’s beneficial to grasp how these anticoagulant medications work. We’ll examine the functioning of the three main types of anticoagulants.
Direct Oral Anticoagulants (DOACs)
Direct oral anticoagulants (DOACs) are a group of anticoagulant medications that directly target specific clotting factors, providing a more predictable anticoagulant effect with fewer interactions. Examples of DOACs include:
Dabigatran
Apixaban
Edoxaban
Betrixaban
These drugs are often prescribed as an alternative to other anticoagulant medications, particularly when warfarin is not a viable option.
The primary advantage of DOACs over other anticoagulants is that they do not require frequent laboratory monitoring and can be administered on a regular basis. They function by attaching to specific clotting factors, such as thrombin, and inhibiting their role in the clotting process. This makes them effective in treating blood clots and preventing their formation after certain medical procedures.
Vitamin K Antagonists
Vitamin K antagonists, such as warfarin, are another type of anticoagulant that works by disrupting the production of clotting factors, which in turn affects blood flow. Warfarin inhibits the utilization of vitamin K in the clotting process and is one of the most widely used anticoagulant medications. However, unlike DOACs, vitamin K antagonists require regular monitoring and dose adjustments to ensure their effectiveness and minimize potential side effects.
Vitamin K antagonists prevent the functioning of vitamin K epoxide reductase (VKOR). This enzyme is essential for the gamma-carboxylation of several factors, such as:
factors 2
7
9
10
protein C
protein S
Due to their specific mechanism of action, vitamin K antagonists may not be suitable for all patients, and in some cases, other anticoagulant options, such as DOACs or heparin, may be more appropriate.
Heparin
Heparin is a fast-acting anticoagulant that is utilized in numerous medical circumstances, such as during surgeries and in hospitalized patients, to prevent clot formation in blood vessels. It is available in several forms, including unfractionated heparin and low molecular weight heparin (LMWH).
The mechanism of action of heparin involves forming complexes with antithrombin 3, resulting in the inactivation of various clotting factors.
Although heparin is effective in preventing the formation of blood clots, it can also lead to potential side effects and complications, such as bleeding, allergic reactions, and interactions with other medications and supplements. It is crucial for patients taking heparin to consult their physician and access available resources to better understand and manage their anticoagulant treatment.
Indications for Anticoagulant Therapy
Anticoagulant therapy is typically prescribed for conditions such as atrial fibrillation, venous thromboembolism, and post-heart valve replacement in order to prevent blood clots and lessen the risk of stroke or heart attack. The choice of anticoagulant medication depends on the specific condition being treated and individual patient factors, such as age, weight, and medical history.
We’ll examine the circumstances that necessitate anticoagulant therapy and the specific anticoagulants used for each ailment in greater detail.
Atrial Fibrillation
Atrial fibrillation (AFib) is an irregular and often rapid heart rhythm that can result in various symptoms and complications.
For patients with atrial fibrillation, anticoagulation is vital to reduce the risk of stroke and systemic embolism. Commonly prescribed anticoagulants for atrial fibrillation include direct oral anticoagulants (DOACs), vitamin K antagonists, and heparin, including low molecular weight heparin (LMWH).
Venous Thromboembolism
Venous thromboembolism (VTE), including pulmonary embolism, is a medical condition in which a blood clot forms in a vein, typically in the deep veins of the legs, and can block the flow of blood.
Anticoagulation is the recommended treatment to treat blood clots and prevent developing blood clots in the form of venous thromboembolism, reducing the risk of recurrence. The anticoagulants used to treat VTE include direct oral anticoagulants (DOACs), vitamin K antagonists, and heparin.
Post-Heart Valve Replacement
Post-heart valve replacement patients may require anticoagulation therapy to prevent clot formation on the artificial valve. The choice of anticoagulant medication depends on the specific type of valve replacement and individual patient factors.
Commonly prescribed anticoagulants for post-heart valve replacement include direct oral anticoagulants (DOACs), vitamin K antagonists, and heparin.
Precautions and Interactions with Anticoagulants
Anticoagulants can interact with other drugs, foods, and supplements, which may require careful monitoring and dose adjustments to minimize risks. These interactions can potentially increase or decrease the effectiveness of the anticoagulant medication, leading to complications such as excessive bleeding or clot formation.
We’ll investigate the various types of interactions and the precautions necessary when using anticoagulants.
Drug Interactions
Interactions with other drugs can boost or lessen the effectiveness of anticoagulants, potentially causing complications. Identifying and avoiding potentially dangerous medication combinations is a key step towards ensuring safe and effective anticoagulation therapy.
Online tools such as WebMD’s Drug Interaction Checker and Drugs.com’s Drug Interaction Checker can help patients and healthcare providers identify and prevent dangerous medication interactions.
Food and Supplement Interactions
Food and supplement interactions can affect the efficacy of anticoagulants, particularly vitamin K antagonists like warfarin. For example, individuals taking warfarin should be mindful of foods that are high in vitamin K, as they can interfere with the drug’s effectiveness.
Additionally, consuming alcohol and grapefruit juice while taking warfarin may increase the risk of bleeding complications.
Monitoring Anticoagulation Therapy
Consistent monitoring of anticoagulation therapy is necessary to maintain optimal dosing and minimize potential side effects. This is usually done by measuring the International Normalized Ratio (INR) for patients on warfarin therapy, which helps determine the clotting capacity of the blood and ensure the anticoagulant is operating within the desired therapeutic range.
In certain circumstances, regular blood tests, such as activated partial thromboplastin time (APTT) and anti-factor Xa level, may also be used to monitor anticoagulation therapy.
For more info, visit Updates in Anticoagulation Therapy Monitoring.
Managing Missed and Extra Doses of Anticoagulants
To maintain therapeutic levels and prevent complications, it’s imperative to manage missed and extra doses of anticoagulants appropriately.
If a dose is missed, it should be taken as soon as possible, but if it is not remembered until the following day, the missed dose should be skipped, and the next dose should be taken as normal.
In the event of an extra dose, it is recommended to seek medical counsel.
Potential Side Effects and Complications

Anticoagulant therapy can lead to side effects and complications, such as common side effects, bleeding risks, and severe bleeding that necessitates reversal strategies. Being cognizant of these potential issues and monitoring for any signs of complications while undergoing anticoagulation therapy is crucial.
We’ll scrutinize the potential side effects and complications tied to anticoagulant medications.
Common Side Effects
Common side effects of anticoagulants may include:
Bruising
Bleeding gums
Nosebleeds
Nausea
Vomiting
Diarrhea
Heartburn
Rash
Itching
Hair loss
Dizziness
Headaches
When taking anticoagulant drugs.
Being aware of these side effects can help patients better manage their anticoagulation therapy and seek medical attention if necessary.
Bleeding Risks
Bleeding risks associated with anticoagulants can be influenced by patient-related factors, such as age, gender, weight, and other medical conditions, as well as the specific anticoagulant used.
Research has indicated that warfarin carries a higher risk of significant bleeding than direct oral anticoagulants. This indicates that it should be administered carefully and monitored closely. It is essential for both patients and healthcare providers to be aware of these risks and monitor for any signs of bleeding complications during anticoagulation therapy.
Severe Bleeding and Reversal Strategies
Severe bleeding events may require reversal strategies, including the use of specific reversal agents or blood products. In cases requiring prompt reversal of anticoagulation, the first action is to immediately cease administering the anticoagulant.
Other measures that may be implemented in significant and life-threatening bleeding scenarios include:
The use of activated charcoal within 2 hours of the last dose of anticoagulant
Hemodialysis
Red blood cell transfusion for anemia
Platelet transfusion in cases of thrombocytopenia
Surgical or endoscopic intervention
These measures can help manage and treat bleeding effectively.
Personalized Anticoagulation Treatment Options
Personalized anticoagulation treatment options include:
Personalized warfarin therapy protocols
Non-vitamin K antagonist oral anticoagulants (NOACs)
Pharmacogenetic information for commonly used antiplatelet medications such as clopidogrel
These options consider individual patient factors, preferences, and medical conditions to determine the most appropriate choice.
Knowledge of these personalized treatment options can assist patients and healthcare providers in making more informed choices regarding anticoagulation therapy.
Patient Resources and Support
Patient resources and support, such as educational materials and anticoagulation clinics, can help patients manage their anticoagulation therapy and minimize risks. These resources include:
The NHS NPSA oral anticoagulant therapy patient information pack
Education and information provided by healthcare professionals
Patient financial assistance programs
Patient education materials and resources from reputable sources such as the American Society of Health-System Pharmacists (ASHP) and the Anticoagulation Forum
Anticoagulation management services offered by healthcare institutions
Mobile apps and tools for managing anticoagulant therapy
Elsevier’s resources for anticoagulant therapy education in home health care
Summary
In conclusion, anticoagulant medications play a vital role in the prevention and treatment of blood clots and associated complications. Understanding the different types of anticoagulants, their mechanisms of action, indications, potential side effects, and interactions is crucial for patients and healthcare providers to make informed decisions about anticoagulation therapy. With the help of personalized treatment options and patient resources, individuals can take control of their anticoagulation therapy, minimize risks, and lead healthier lives.
Frequently Asked Questions
What are examples of anticoagulants?
Examples of anticoagulants are apixaban, dabigatran, edoxaban, rivaroxaban and warfarin.
What are the 4 most common anticoagulants?
The four most common anticoagulants are rivaroxaban (Xarelto), Dabigatran (Pradaxa), apixaban (Eliquis) and edoxaban (Lixiana). These direct factor Xa inhibitors block the factor Xa needed to make a clot, and are used to treat and prevent blood clots and stroke.
Is anticoagulant the same as blood thinner?
Anticoagulants, also known as blood thinners, are medicines used to prevent the formation of blood clots, reducing the risk of heart attack and stroke. They work by interrupting the process involved in clot formation, but do not actually make the blood thinner. Examples include low-molecular weight heparin, fondaparinux, warfarin, aspirin, and clopidogrel.
Is aspirin an anticoagulant?
Aspirin is an antiplatelet medicine, not an anticoagulant, that helps prevent the formation of clots in the arteries of the heart and brain. As it interferes with clotting, it may also cause some side effects such as bleeding into the brain or stomach.
How do vitamin K antagonists, such as warfarin, work?
Vitamin K antagonists such as warfarin prevent the production of clotting factors in the body, thereby inhibiting blood flow.